In 2019 a Novartis drug called Zolgensma got approved and made huge headlines. The headlines were less about the fact that this one time treatment can treat spinal muscular atrophy (a condition occurring in 1 out of 10,000 newborns and limiting their life to often mere two years) but about it being the most expensive drug ever.
In the United States the list price of Zolgensma stands over 2 million USD. The one time treatment is a so-called gene therapy that injects a virus aimed at fixing the failed or mutated gene responsible for motoric muscle functions. While this treatment is good news for many patients, it also fueled the debate on the ethics of high drug prices.
I would like to provide a few fresh, not fully reflected, and hopefully provoking thoughts for the new year on what policy makers should keep in mind when aiming to control drug prices.
So why don’t we just cap the prices per drug?
2 million Dollar per patient is definitely a crazy high amount. The reason why it can’t be offered much cheaper right now is that there are (fortunately) not that many patients that actually need this treatment. The drug manufacturer has a very small target audience they can charge for this treatment of a rare disease. From that small pool of people they need to recoup their development costs for this drug, make up for totally failed projects, and make shareholders happy with a profit margin.
This sounds cruel – So why don’t we have stronger laws on capping such excesses? If we legislate a maximum cap to how much a drug per patient is allowed to cost, we will end up with pharmaceutical research aimed at treating and curing common diseases and patients with rare diseases will have a bleak future.

Why are there so often drugs that are similar to already existing drugs and don’t focus on curing diseases we can’t cure or treat yet?
Medical research is unfortunately a shotgun. When starting to develop a molecule or target a genetic defect you never really know where you end up. On average, only one of every 5,000-10,000 substances synthesized in research facilities will make it successfully through all stages of product development to become an approved drug. Many projects and even entire biotech companies fail to bring even one product to the commercial stage. Investing in life sciences requires a very healthy appetite for risk, and hence an incentive scheme that rewards those able to create value with their inventions is required. By the time a medical drug reaches the regular patient, an average of 12.5 years will have elapsed since the first discovery of the new active substance. The total investments needed to get to one active substance that can be accessed by a patient is around two billion Euros.
Why is delinkage is a bad, very bad, idea?
There are big proponents within the World Health Organization and some southern European governments to de-link the research and production of medical drugs. Supporters of this so-called delinkage support publicly funded R&D of drugs and private companies merely charging for their production costs plus a modest markup. This semi-planned pharma economy should frighten all those who are still waiting for medical innovations to cure their or their loved ones from medical conditions. Medical innovation (or to be more precise the lack of it) in planned economies such as the Soviet Union is a solid benchmark of why this is a bad idea. Research funding has been politicized in such systems and only funneled into pet projects of apparatchiks or (in the best case) to very common diseases the majority of voters are interested in.
Side note: The Soviet Union put in a lot of effort to develop cutting-edge doping drugs for their Olympic athletes but neglected researching actual cures. An example is the story of a Russian scientist who smuggled in a drug with the help of Mayo Clinic practitioners to treat his daughter’s tuberculous meningitis was even sentenced to death for being in contact with an American scientist.

So how can things stop getting more expensive?
Critics of the innovative pharmaceutical industry make often the point that pharma has an incentive to not fully cure patients as they only make money with sick patients. The same argument can be made about hospitals and outpatient doctors. There are historic capitation examples in which doctors only get paid per healthy patient month (I was told by someone very smart that this used to be the case in ancient Chinese villages). These concepts obviously work much better in a super-low-tech health system or for the reimbursement of providers only. Adding pharmaceutical research into this equation makes things definitely hard; but not impossible.

So would it be possible to have fully integrated healthcare companies that are providers, payers, and pharma industry at the same time?
A rather crazy thought experiment: I just googled vertical integration pharmaceuticals and insurance and surprisingly couldn’t find much. My healthcare management textbook told me a decade ago that integrating (or collaborating) with pharma would be called a diagonal collaboration as pharma and med tech are often not even seen as a proper part of the health system. A vertically integrated healthcare company owning drug patents and having patent cross license agreements with similar companies would have a higher incentive to provide its patients/insurance population with all drugs it has access to. Given the growing importance of health data both in treating patients (patient value chain) but also finding cures could be massively leveraged in such an integrated organization. The main profits would be generated through insurance premiums and drug sales to markets the insurance is not active in or to competitors.
This could be an interesting market response to realigning incentives in private healthcare and healthcare in general. The biggest roadblocks and reasons why this has not happened yet are:
- Insurance multinationals are insurance companies and more banks than healthcare companies.
- Pharma multinationals are research companies and not financial institutions.
- Bringing these two worlds together is rather something for innovative entrepreneurs of the Bezos type. Paypal brought together email and bank wire, Skype combined your computer and international calls, Amazon online shopping and fresh food in your fridge, many more examples of disruption of legacy industries caused by an outsider can be added here…
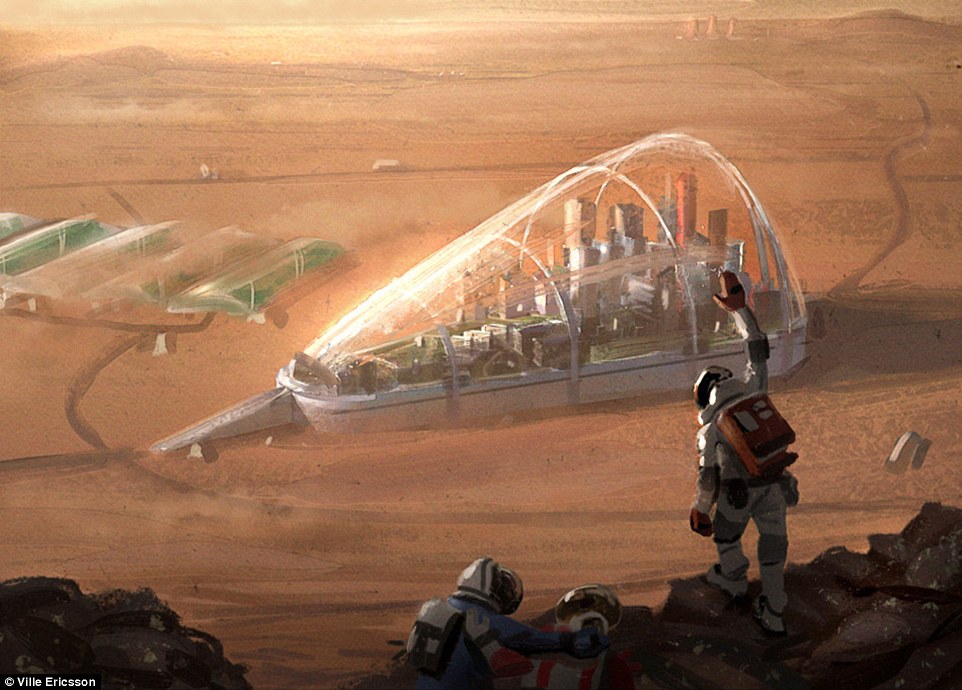
- Given the fact that that most countries have a very strict and prospective regulatory framework of healthcare, does not really permit such an integrated company to reach any significant mass of patients. A really big market such as Germany, the UK, Japan or a handful of large US States would have to allow disruption of their own rigid health systems and overcome the dichotomy of health sectors (provider, payer, industry). Exciting for science fiction books and thought experiments but right now unfortunately more realistic for a future lunar or Mars colony than to happen in a developed country.
Will the next big thing come out of a garage lab?
I recently watched the very entertaining Netflix documentary series Unnatural Selection that shows both the significant advances of gene therapy by established pharma companies and some outlaw biohacker activists that try to democratize biotech research through their garage labs. While most of these biohackers seem to be overly optimistic of their chances to develop effective cures and genetic improvements, one should not reject the possibility of disruption within the biotech industry.
The big consumer-reaching advances of the computer and software industry happened eventually in Californian and New Mexican garages and not in the labs of IBM or GE. Gene editing techniques such as CRISPR bring a lot of hope to patients and families struggling with genetic diseases. And first advances with this technology in agriculture and animal health suggest that treatments can be developed in relatively small and inexpensive labs and research environments.
So there’s a possibility that the competition density in the biotech industry will intensify and market entry barriers be lowered due to gene editing technologies. At the same time regulatory barriers and approval requirements need to adopt to these technologies, allow them, and take into account that too high barriers will keep competition low and hence prices for new treatments high.
Quick and easy one to save Billions in 2020: Scrap value added and all sales taxes from prescription medicine. In some countries this would lead to a reduction of drug prices by 25%! It is also more than sad that some developing countries still levy tariffs on imported innovative medicines.
Please feel free to chip in to this debate. It is important to keep an open mind and find new ways to fund innovative medicine. At the same time it is important to stick to the realities of medical research and innovation.
A less futuristic but more public policy oriented paper on ‘The Consumer Case for Intellectual Property’ authored by me can be found here.